Medical billing and coding audits are necessary checkups to ensure a provider’s billing claims and coding documentation meet medical billing compliance. Certified billing auditors inspect patient charts and billing records to guarantee the use of correct codes that match conditions and care. Like routine physicals catching health problems early, audits diagnose issues in billing, allowing providers to correct course.
Audits are important as they reveal improper coding, incomplete documentation, missed charges, and noncompliance with reimbursement guidelines. This helps strengthen a provider’s revenue cycle by correcting errors proactively before they can lead to denied claims or penalties for incorrect billing. Regular comprehensive audits are advantageous as they ensure proper coding, completeness of records, optimal reimbursement, compliance with payer policies, and overall financial health.
Timely Bills Solutions works as a professional medical billing audit services company. Medical billing and coding is complex work full of pitfalls for error, calling for vigilant oversight. Therefore, our medical coding audit and compliance services provide this monitoring, serving as a safety net that preserves the integrity of the entire medical claims billing process.
The experienced billing auditors at Timely Bills Solutions, take a magnifying glass to documentation, coding choices, and the submitted claims to unveil inaccuracies and illuminate opportunities for billing cycle improvement. Our findings steer healthcare facilities toward error-free medical coding and full revenue capture.
Just as crucial, our high quality medical billing audit program heads off billing compliance violations and fraud that lead to fines, penalties and damaged integrity. Our audit service is thus a fundamental pillar upholding clinical, financial, and regulatory excellence.
Timely Bills Solutions provider credentialing process is not just a routine procedure, but a validated and certified process that ensures the highest standards of compliance. We have achieved up to 98% success rate of getting providers approved in premium payer networks with maximum privileges in their specific specialties. The process typically includes the following steps:
Our credentialing process begins with an in-depth survey conducted by our credentialing specialists. This process involves comprehensive interviews with providers, gathering essential data such as license numbers, educational history, demographics, and professional background.
Our medical credentialing services guide providers in strategically choosing insurance partners aligned with their practice goals and license type, while also finalizing insurance panels based on practice location.
We take care of CAQH application submissions, manage ProView accounts, and keep credentials current for smooth primary source verification. We also assist with payer credentialing submissions, ensuring quick insurance panel integration and accurate profiles that enhance network engagement and the quality of patient care.

We do medical coding audits for all types of medical records, including inpatient, outpatient, profee, and home health.
We do medical billing audits for all types of claims, including Medicare, Medicaid, commercial, and self-pay.
We improve your cash flow by auditing your aged claims for errors and refiling denied claims with our collection aging audit.
We audit Medicare patient charts, ensuring every dollar billed is justified and compliant, so your practice gets fully and fairly paid.

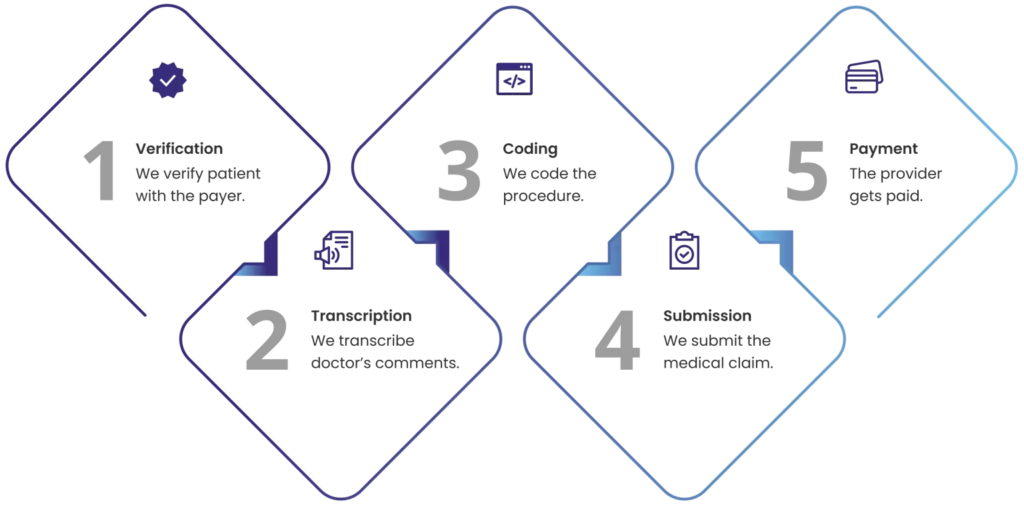
Medical billing can be prone to errors, delays, and inefficiencies that affect your cash flow and profitability. Timely Bills Solutions billing associates streamline your clinic’s billing process by taking care of the entire RCM with real-time reports and analytics.