Our clearinghouse provides real-time updates on the status of sent files, ensuring transparency and accountability.
When secondary insurance comes into play, Timely Bills Solutions streamlines the process, minimizing delays and maximizing reimbursements.
Get a consolidated view of all your clearinghouse activity. Transaction summaries help you stay organized and make informed decisions.

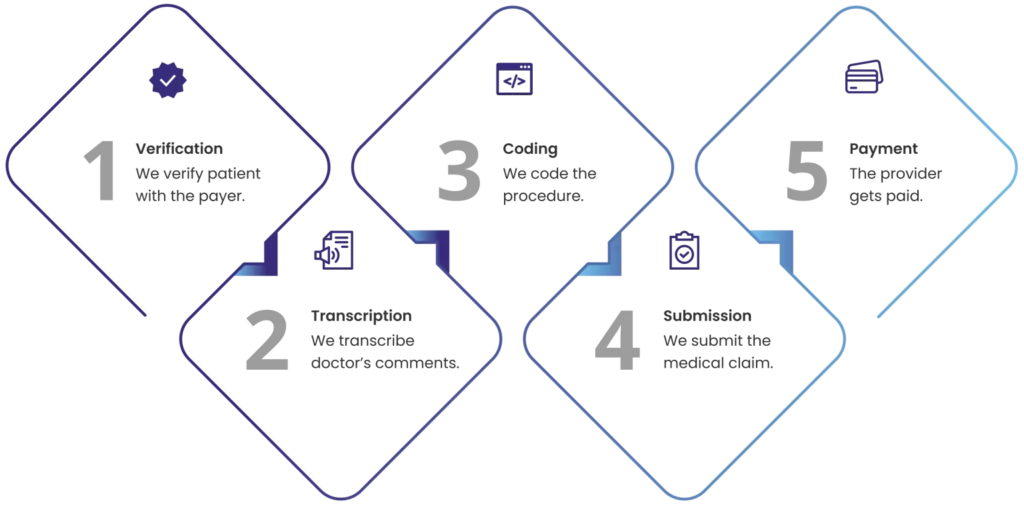
Medical billing can be prone to errors, delays, and inefficiencies that affect your cash flow and profitability. Timely Bills Solutions billing associates streamline your clinic’s billing process by taking care of the entire RCM with real-time reports and analytics.