Credentialing, also known as insurance credentialing or doctor credentialing, is a process that verifies the qualifications, skills, and legitimacy of a healthcare providers. This process ensures that the provider has necessary licenses, certifications, and education to provide healthcare services to patients.
Only a credentialing provider is eligible to receive payments from the payer and work in compliance with the state and federal regulations. Medical credentialing authorizes physicians to practices in a specific facility and be included in insurance networks like CMS/Medicare, Medicaid, Aetna, Cigna, Humana, UnitedHealthcare, and Blue Cross Blue Shield.
As a provider, you want fast credentialing so as to start practicing and billing (legally and ethically). But credentialing is a complex process that involves a lot of documentation and verification at different stages by the insurance network. This means a single mistake can result in denials and wastage of resources such as time and money.
BellMedEx medical billing company offers the best healthcare credentialing solutions. Our professionals handle all the tasks for you, from primary source verification to enrollment in premium payer networks. We do all of this in minimal time and budget.
Timely Bills Solutions provider credentialing process is not just a routine procedure, but a validated and certified process that ensures the highest standards of compliance. We have achieved up to 98% success rate of getting providers approved in premium payer networks with maximum privileges in their specific specialties. The process typically includes the following steps:
Our credentialing process begins with an in-depth survey conducted by our credentialing specialists. This process involves comprehensive interviews with providers, gathering essential data such as license numbers, educational history, demographics, and professional background.
Our medical credentialing services guide providers in strategically choosing insurance partners aligned with their practice goals and license type, while also finalizing insurance panels based on practice location.
We take care of CAQH application submissions, manage ProView accounts, and keep credentials current for smooth primary source verification. We also assist with payer credentialing submissions, ensuring quick insurance panel integration and accurate profiles that enhance network engagement and the quality of patient care.

Enjoy the advantage of first-preference reimbursement rates, maximizing your financial rewards. This means you get paid more for the same services, increasing your profitability and satisfaction.
Our streamlined approach not only wins you contracts but also secures vital privileges. You will be able to participate in innovative programs, as well as get incentives for quality performance.
You'll be prepared to bill from day one, saving you precious time. You will receive a unique provider identification number (PIN) that allows you to submit claims electronically and track them online.
Our advocacy ensures insurance companies stand by you, supporting your needs. We negotiate on your behalf and resolve any issues that may arise, ensuring you get paid fairly and promptly.

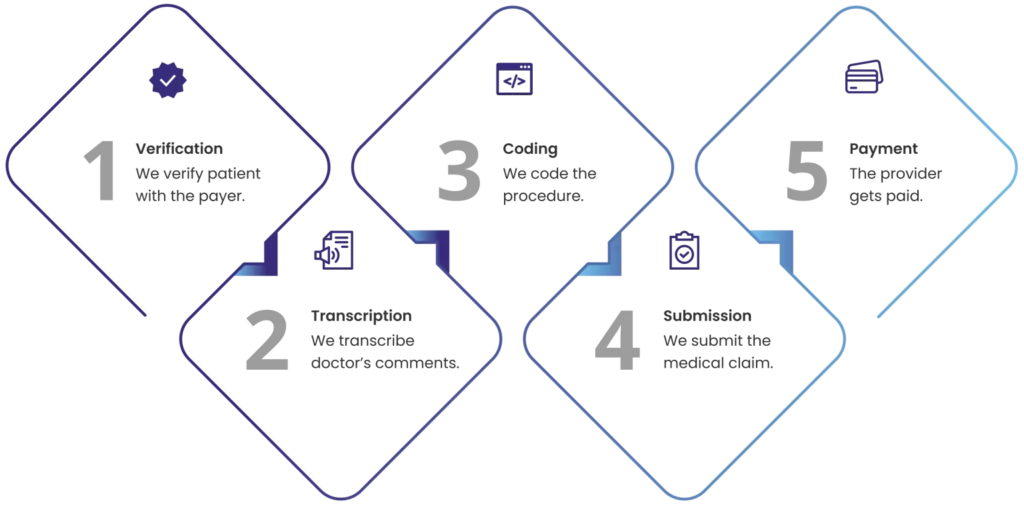
Medical billing can be prone to errors, delays, and inefficiencies that affect your cash flow and profitability. Timely Bills Solutions billing associates streamline your clinic’s billing process by taking care of the entire RCM with real-time reports and analytics.